When someone hears “cancer,” a knot in the heart tightens — fear, uncertainty, and a thousand questions flood in. What if the treatment is generic, doesn’t fit you? The game has changed. Today, a skilled cancer doctor doesn’t just create a default treatment plan. ” They turn to precision oncology, genomic profiling, liquid biopsy, AI in cancer treatment, and more, making cancer treatment highly accurate and personalised.
If you’re reading this because you or someone you love is facing cancer, let’s walk through how modern oncologists are rewriting the playbook — and how that helps you.
Precision Oncology
The concept of precision oncology is that, instead of treating all tumours of a given organ the same way, doctors delve deeper into each tumour’s molecular structure and genetic factors.
Example: Two patients both have lung cancer. One tumour has a specific EGFR (epidermal growth factor receptor) mutation; the other doesn’t. With genomic testing, the oncologist can select a drug that targets the mutation for the first patient, while the second patient may need a different path.
Why it matters for you: If you visit a competent cancer doctor in Kolkata, ask about tumour profiling. It gives you more information and better odds of choosing the right treatment early.
Genomic Profiling
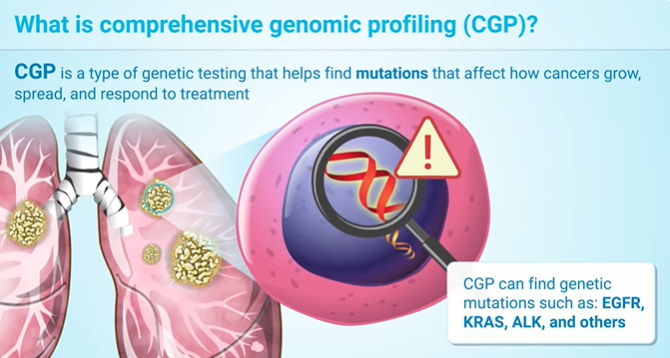
Genomic profiling is the process of scanning the tumour profile to find where it went wrong. This isn’t futuristic fiction — studies show that Comprehensive Genomic Profiling (CGP) can identify actionable targets in 81 % of advanced-cancer cases in one study.
| Tool | What it examines | Why it matters |
| DNA sequencing (NGS) | Tumour’s DNA changes (mutations, gene fusions) | Helps pick targeted drugs |
| Transcriptomics / RNA | Which genes are active | May show drug resistance or immune-escape |
| Biomarkers like TMB, MSI | “How many mutations?” / “How unstable?” | Helps decide immunotherapy eligibility |
Example: A breast cancer patient’s test shows “HER2 positive”. That tells the doctor they can use a “targeted therapy” instead of generic chemo.
Why it matters: If you’re choosing treatment with a cancer doctor, asking whether genomic profiling has been done (or should be) can make a big difference.
Targeted Therapy
After the profiling is done, doctors can use targeted therapy , which includes drugs that aim exactly where the tumour is vulnerable. The National Cancer Institute explains this as treatments that interfere with proteins controlling how cancer cells grow, divide, and spread.
Example: In Chronic Myelogenous Leukaemia (CML), most patients have the BCR-ABL gene. Drugs like imatinib target exactly that. In solid tumours, similar logic applies (though often more complex).
Note: Targeted therapy is not magic. Tumours can develop resistance. But starting with a tailored option improves odds.
Immunotherapy Advancements
Instead of fighting cancer for you, immunotherapy fights cancer with you — by training your immune system. Recent reviews show major strides in this field.
Example: Immune checkpoint inhibitors block tumour tricks that hide the tumour from immune cells. Other therapies use engineered immune cells (CAR-T, CAR-NK) or cancer vaccines.
Why it matters: When you see a “modern” cancer doctor in Kolkata, ask how immunotherapy fits your case. Some tumours respond especially well when profiling shows a “high mutational burden” or certain markers.
Liquid Biopsy

Traditionally, doctors take a sample of tumour tissue (a biopsy). But what if you could catch tumour DNA in blood or other fluids? That’s a liquid biopsy. A recent review calls it “minimally invasive and suggests that it holds significant potential for future applications.”
Example: After surgery, doctors monitor for tiny amounts of tumour DNA in the bloodstream. If it shows up, treatment adjustments can happen before imaging detects relapse.
Why it matters: With less pain, fewer complications, and faster turnaround, liquid biopsies allow real-time monitoring. Ask if your clinic has access to this for follow-up.
AI in Cancer Treatment & Digitisation in Oncology
Here’s where things get futuristic. AI helps oncologists crunch massive data: images, genomics, patient history. Studies show AI can aid in diagnosis, treatment planning, and prognosis prediction.
Example: An AI tool analyses pathology slides and picks patterns that even expert humans miss. Another integrates genomics, imaging, and labs to suggest treatment options (a “decision-support” engine).
Digital health in oncology includes tele-oncology (remote consultation), wearable monitoring of side effects, and electronic symptom tracking. This connects you wherever you are.
Why it matters: A cancer doctor in Kolkata utilising these tools isn’t just following standard protocol—they’re leveraging data, personalisation, and continuous monitoring. That raises your chances of better outcomes.
Personalised Cancer Care
When we say “personalised cancer care,” we mean combining all of the above: profiling the tumour, picking the right target/immune therapy, monitoring with liquid biopsy, integrating AI and digital tools, and tailoring follow-up.
Example:
- Step 1: Patient comes in, tumour biopsy + blood tests + genomic profiling
- Step 2: The Oncologist uses AI-enabled analytics and tumour board discussions
- Step 3: A tailored plan is created: targeted drug + immunotherapy + digital monitoring
- Step 4: Liquid biopsy is used every few months to watch for relapse trends
- Step 5: Tele-oncology follow-ups, digital symptom tracking, side effects managed proactively
Practical Considerations: What you, as a patient/family, can ask
- Has the tumour undergone genomic profiling? What genes were tested?
- Are there targeted therapy options or immunotherapy based on my profile?
- Could a liquid biopsy help monitor my progress?
- How is digital health (symptom tracking, remote consults) being used in my case?
- What is the backup plan if resistance develops or new mutations emerge?
- How will the multidisciplinary team coordinate (medical oncologist, pathologist, radiologist, geneticist)?
The War Against Cancer Isn’t a Generic Fight Anymore
When you walk into the clinic of Dr. Joydeep Ghosh, a trusted cancer doctor in Kolkata, you will feel like you’re part of the treatment plan. So, ask questions and understand the tech being used. Advancement in cancer treatment means smarter tools — and experts who use them.
To learn more, consult Dr Joydeep Ghosh, a leading oncologist in Kolkata. Call 98755 18968 to book an appointment.
People Also Ask
What is precision oncology, and how does it differ from traditional cancer treatment?
Precision oncology means targeting treatment to the individual tumour’s characteristics (DNA/RNA changes, biomarkers) rather than treating everybody with the same cancer type in the same way. Traditional treatment may use standard chemo or radiation regardless of the tumour’s molecular features.
How does genomic profiling help in cancer treatment?
Genomic profiling examines a tumour’s genetic/biologic changes. It helps oncologists identify mutations, gene fusions, or biomarkers that are “actionable” — meaning there’s a drug or strategy developed for that change. Patients whose treatments are matched by profiling often have better outcomes.
What is a liquid biopsy, and why would I need one?
A liquid biopsy is a blood (or other fluid) test that looks for tumour-derived DNA or cells circulating in the body. It’s less invasive than a tissue biopsy. It can be used to detect early changes, monitor treatment response, or detect relapse before it becomes visible on a scan.
How is artificial intelligence used in cancer treatment?
AI is used in many ways: analysing imaging and pathology slides for patterns, integrating genomics and patient data to suggest therapies, and predicting treatment response or drug resistance. It supports oncologists (not replaces them) to be more precise.
What are the latest advances in immunotherapy for cancer?
Recent advances include better immune-checkpoint inhibitors, cellular therapies like CAR-T and CAR-NK cells, cancer vaccines and combinations of immunotherapy with other treatments. These approaches are improving outcomes even in previously hard-to-treat cancers.



