Behind every brave little fighter, a medical expert is planning every step. For years, pediatric cancer treatment relied on high-dose chemotherapy and radiation, which often affected healthy tissues along with cancerous ones. But with the rise of medical oncology and precision medicine, the treatment process has evolved.
Dr Joydeep Ghosh, a medical oncologist in Kolkata, is redefining how pediatric cancers are treated.
This blog takes a closer look at how pediatric oncology supports children through every stage of cancer care. It explains common childhood cancers and treatment options like chemotherapy and immunotherapy. It also highlights the role of personalised care in long-term healing.
What is Medical Oncology in Pediatric Care?
Medical oncology in children is also called pediatric oncology. It focuses on diagnosing and treating cancer in kids, teens, and young adults.
It is different from adult cancer care. Childhood cancers usually come from early genetic changes. They grow faster and need treatments personalised to a child’s developing body.
Which Childhood Cancers Are Managed by Medical Oncology?
Leukaemia and Lymphoma
Leukaemia and lymphoma are blood cancers and the most common types of pediatric cancer. They can be tricky to detect early because many symptoms may look like common infections or general tiredness in children.
Symptoms:
- Tiredness and weakness
- Pale skin, dizziness, or shortness of breath during normal activity (due to low red blood cells)
- Easy bruising, frequent nosebleeds, or red spots on the skin (from low platelets)
- Fever and frequent infections that are hard to treat
- Bone or joint pain, especially if it causes limping
- Swollen lymph nodes in the neck, underarms, or groin
- Night sweats or itchy skin (especially in lymphoma)
Solid Tumors (Neuroblastoma, Wilms’ Tumor, Sarcomas, Brain Tumors
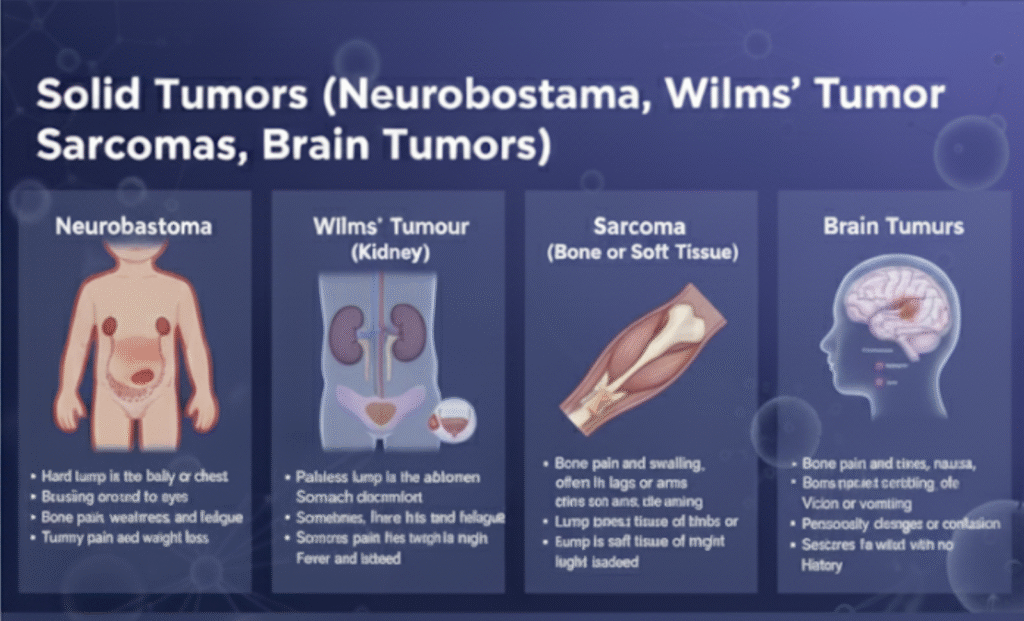
Solid tumours in children form in different parts of the body, like the abdomen, bones, kidneys, or brain. They don’t always cause pain at first, so a new lump or discomfort should never be ignored.
Specific signs to watch for:
- Neuroblastoma
- Hard lump in the belly or chest
- Bruising around the eyes
- Bone pain, weakness, and fatigue
- Tummy pain and weight loss
- Wilms’ Tumour (Kidney)
- Painless lump in the abdomen
- Stomach discomfort
- Sometimes, there is blood in the urine
- Fever and tiredness
- Sarcoma (Bone or Soft Tissue)
- Bone pain and swelling, often in the legs or arms
- Lump in soft tissue of limbs or chest
- Pain that wakes the child at night
- Brain Tumours
- Morning headaches, nausea, or vomiting
- Vision or balance issues
- Personality changes or confusion
- Seizures in a child with no previous history
Get expert pediatric cancer care with Dr Joydeep Ghosh, a medical oncologist in Kolkata. Schedule your appointment.
Common Treatment Options in Pediatric Oncology
Chemotherapy
What it is & how it works
- Chemotherapy uses powerful drugs to kill cancer cells. These drugs travel through the bloodstream and reach cancer wherever it is in the body (systemic therapy). Sometimes, they are delivered specifically to one area (regional therapy), such as into the brain or spine.
- Treatment is given in cycles: there’s a phase of drug administration followed by a rest/recovery period so the child’s body can heal.
How is dosing different in children
- Children are not just “small adults.” Their bodies process drugs differently depending on their age, weight, body surface area, and how mature their organs are.
- Protocols are designed to balance killing cancer cells and minimising damage to healthy cells for long-term health.
Common side effects & long‑term concerns
- Short‑term side effects: nausea, vomiting, hair loss, mouth sores, tiredness, risk of infections because blood cell counts drop.
- Serious or specific side effects depend on which chemotherapy drugs are used. For example, doxorubicin can affect the heart, and some drugs damage hearing or the kidneys.
- Long‑term effects (often called “late effects”): delayed growth, possible problems with how the heart, lungs or other organs work; sometimes risk of second cancers, fertility issues, or learning difficulties.
Targeted Therapy and Precision Medicine
What is it & why is it important
- These therapies are developed to zero in on specific genetic changes or “weak spots” in cancer cells.
- Because they are more selective, they cause fewer side effects compared to traditional chemotherapy.
Limitations & what to watch for
- Not every cancer has a known target or mutation that can be treated with these drugs. Some cancers still need traditional chemotherapy or combined treatments.
- Resistance can develop, meaning the cancer might adapt, and the targeted drug may stop working over time.
- Side effects are still possible, though often milder. Effects depend on the exact drug and the patient. Monitoring is required.
Immunotherapy
What are these & how do they help
- Immunotherapy is a way to help the body’s own immune system recognise and destroy cancer cells. It “turns on” immune defences that often fail to detect cancer.
- Two important types in pediatric use:
- Checkpoint inhibitors: These are drugs that block the “brakes” the cancer uses to hide from immune cells. Once those brakes are removed, the immune system can attack the cancer.
- CAR‑T cell therapy: Doctors start by taking T-cells from the child’s blood. T-cells are a type of immune cell that helps fight infections. In the lab, these T-cells are genetically modified so they can recognise a special marker found on cancer cells. The modified T-cells are then multiplied (grown in large numbers) in the lab. After that, the modified cells are infused back into the child’s body.
- Checkpoint inhibitors: These are drugs that block the “brakes” the cancer uses to hide from immune cells. Once those brakes are removed, the immune system can attack the cancer.
Once inside, they seek out and attack the cancer cells carrying that specific marker. It is used especially for certain kinds of leukaemia that have relapsed or not responded to other treatments.
Challenges & risks
- Side effects: immunotherapy can trigger immune over‑reactions (for example, fever, inflammation, organ effects) because the immune system becomes highly active. Monitoring in hospital or under medical supervision is essential.
- Cost & accessibility: CAR‑T therapy is complex, expensive, and requires special facilities. Not always available everywhere.
Individualised Care Pathway
Every child is different. That’s why pediatric oncology does not use a one-size-fits-all approach. Instead, it builds a treatment roadmap based on the child’s diagnosis, age, risk level, and health. This ensures the treatment is both effective and gentle. It helps the child fight cancer without compromising their development.
Diagnosis, Staging, and Risk Stratification
Before starting treatment, doctors need to understand the cancer completely. This step is called diagnosis and staging.
To do this, several tests are done:
- Imaging scans (like MRI or CT)
- Blood tests
- Bone marrow biopsies
- Lumbar punctures (spinal tap)
Outcomes, Survival, and Long-Term Follow-Up
Survivorship Clinics & Late Effects Monitoring
- Even after treatment, care continues.
- Regular check-ups monitor heart, bones, and brain health.
- These visits check for survivorship and late effects in children.
- Emotional and school support is part of the follow-up.
Rehabilitation, School Reintegration, and Vaccinations
- Physical therapy helps regain strength.
- Schools and hospitals work together for a smooth return to class.
- Missed vaccines are given later under medical advice.
Case Study
Patient Information:
- Age / Gender: 10 years old / Male
- Health Concern: T-cell Acute Lymphoblastic Leukaemia (T-ALL) relapse with multiple lymphadenopathies, no discomfort.
- Initial Treatment: Induction chemotherapy (which did not result in remission).
Diagnosis:
- Relapsed T-ALL (T-cell Acute Lymphoblastic Leukaemia).
Treatment Provided:
- CD7 CAR-T Cell Therapy: The patient received CD7 CAR-T cells from his father as the donor.
- Outcome After CAR-T Therapy: Achieved complete remission (CR).
- Allogeneic Hematopoietic Stem Cell Transplantation (allo-HSCT): Thirty days after the CAR-T cell infusion, the patient received allo-HSCT with his father as the donor.
Outcome / Result:
- The patient achieved complete remission (CR) and has maintained long-term survival, with a leukaemia-free survival (LFS) of more than 3 years.
Conclusion:
This case supports the use of CD7 CAR-T therapy followed by allo-HSCT as an effective and safe treatment for relapsed/refractory T-ALL, leading to long-term survival and a good prognosis.
(Source)
Healing with Heart and Science
Pediatric oncology isn’t about treating cancer. It is about supporting a child’s growth, healing, and success.
With tools like targeted therapy in children, childhood cancer immunotherapy, and personalised care, young patients now have better chances than ever. With the right care team, even the toughest battles can lead to a brighter tomorrow.
Book an Appointment
Book a consultation with Dr Joydeep Ghosh, a medical oncologist in Kolkata and give your child the care, comfort, and advanced treatment they deserve.
People Also Ask
- What is the success rate of childhood cancer treatment?
Many childhood cancers, like leukaemia, have success rates over 80% when treated early.
- Is chemotherapy safe for kids?
Yes. Pediatric chemotherapy is given in safe doses with strong support.
- What is CAR-T therapy for pediatric cancer?
It uses a child’s immune cells, modified to attack cancer. It’s used in challenging cases.